Any parent who loses a child here on Earth carries a certain amount of insensible guilt. God gives us a child, and our first obligation is to try to keep that child safe in a world that is full of hazards, at almost every age. The challenge, which is to love, educate and teach that child not only to live in the world but to flourish in it, is a large one. So, we look for the best schools, the best churches and the best doctors, and even then sometimes, we miss something, or something somewhere goes awry.
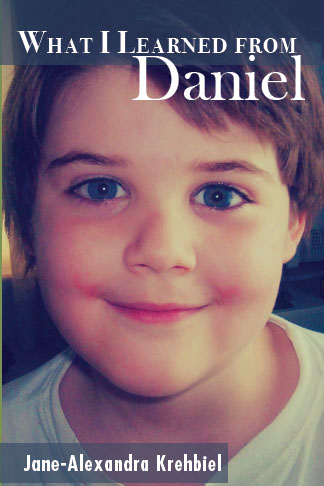
I remember the day Daniel died as if it were yesterday. One moment my extremely bright youngest son was talking to me, and the next moment, I heard a crash in the bathroom. I found him in a full cardiac arrest, and I began CPR. I asked other family members to call 911 and ask for the medical helicopter for a child in a full cardiac arrest. I remember wondering what could possibly have done this to my healthy child who'd had a clean physical just a couple of weeks before.
Despite the sheriff's office using the AED and a very competent team of professionals from the helicopter, we were not able to restart Daniel's heart at any point during his code. This has always bothered me because I have been lucky. In the hospital setting or outside it, I have never had a patient who received immediate CPR for a witnessed cardiac arrest, not respond. (Although in all honesty, I might have gotten them back only to have them die later that day.) It has always bothered me that Daniel did not respond in any way to the CPR. It was as if he were gone when he hit the floor.
As longstanding readers will recall, initially his autopsy was very good. His coronary arteries were as clean as a whistle, which is not true of a number of 12 1/2 year old American children. His brain was normal, although they were some incidental findings that did not cause death. Pathologists were left with a healthy child who was clearly dead. Daniel was made a teaching patient, and different pathology teams at a world class teaching hospital each took a crack and what might have happened. Because Daniel had entered the bathroom, vomited, collapsed and fallen forward, the pathologists felt that this had likely been a sudden arrhythmic death, which is basically a spontaneous disruption of heart rhythm of unknown cause. While toxicology was sent, the doctors used the time to question our family on other cardiac or arrhythmic deaths among our relatives, or other arrhythmic disorders among those who remained living. I shared that we had a fair amount of atrial fibrillation among the over age seventy members of the family, although no one we knew had died in the manner of Daniel. Eventually, because sudden arrhythmic death syndrome or the other diagnosis SUDC, which is sudden unexplained death in childhood, are disorders from a functional problem not a structural one, and nothing of any interest was yielded from toxicology, Daniel's passing was attributed to a sudden cardiac arrest of uncertain etiology, or cause. His DNA and other samples were sent to the Mayo Clinic who was studying whether he might have one of the many identified familial causes sudden cardiac arrest. Some of these are Brugada Syndrome, Wolff-Parkinson-White Syndrome, Long QT Syndrome, Short QT Syndrome, etc. A long time afterward, Mayo Clinic communicated that Daniel did not show evidence of any of the familial arrhythmic syndromes that could be identified from DNA samples at that time. Perhaps he had a syndrome that has not yet been identified, they speculated. (Of course, this began the odyssey of having our remaining children examined and having a preventive cardiac ablation done on one of them.)
Fourteen years later, I am still left with the feeling that I have missed something, and that this is somehow my fault, even to some small degree. Since then, some clues have emerged within the remaining family. There are family members who have erythropoietic protoporphyria (EPP), some with Crohn's Disease and one with cystic fibrosis. All of these disorders are associated with, or can lead to a Vitamin D deficiency. Interestingly, even as a young person, I have been found to have a very low Vitamin D level at intervals. I have also been fairly resistant to having this corrected, requiring relatively large amounts given over a long period of time before it is corrected. How could this be ? I have asked. The answer I get is that some people lack the enzyme to manufacture Vitamin D from sunlight and cholesterol. No one asked whether this could have been a familial issue. Even if it had been, there had not been an association between low Vitamin D levels and sudden arrhythmic death. However, there is now.
Recent studies have shown that people, including children with low Vitamin D levels have a much higher rate of dying from a sudden episode of arrhythmic death. If Daniel had a familial tendency to have low Vitamin D, coupled with a missing enzyme in order to make Vitamin D from sunlight, could this be the missing part of the puzzle ? Physicians do not routinely test for Vitamin D levels, and they don't often check in children. There was no known reason to check, and at the time, no known association with sudden arrhythmic death. It is only now that we know from several recent studies that low Vitamin D is associated with ionic channel disorders which can lead to sudden alterations in the EKG such as the QT interval.
For those of you who have a medical or personal interest in this, this is one of the authoritative articles, which I believe is the easiest to understand.
https://journals.viamedica.pl/kardiologia_polska/article/download/82363/61698
When Daniel died, we had not had history with other family members that indicated that we were all Vitamin D deficient. We all took vitamins, except for Daniel who wouldn't swallow pills and was not sold on taking his chewable Flintstone's vitamin daily. I do so wish I had known this. In 2008, physicians did not suspect that any of us were low in Vitamin D, and perhaps they didn't even know of familial Vitamin D use disorders.
It is my hope that this post reaches someone that it may help. Some of us persist in having low vitamin D levels even when supplemented, and this may require regular monitoring as well as prescription amounts of this vitamin. To simply blindly replace Vitamin D without proper monitoring may be equally dangerous. If you suspect this is an issue for your family, please see your doctor and ask for a Vitamin D blood test.
.png)


.png)











